The CDC’s vaccine advisory committee’s recent decisions could impact how your family gets vaccinated. To help break down what changed and what didn’t, News On 6’s MaKayla Glenn spoke with Dr. Mandy Griffin, a pediatrician at Utica Park Clinic in Tulsa. Click here to view the story online.
The CDC’s vaccine advisory committee just wrapped up two days of meetings, and the decisions could impact how your family gets vaccinated.

Dr. Mandy Griffin, a pediatrician at Utica Park Clinic in Pryor, breaks down what changed and what didn’t.
Q: What was the purpose of this CDC meeting?
“The purpose of the meetings these past two days were to talk about three different vaccines,” Dr. Mandy Griffin said.
The CDC’s Advisory Committee on Immunization Practices, or ACIP, met to vote on key recommendations for the MMRV combination vaccine, the hepatitis B vaccine at birth, and COVID-19 vaccination guidelines.
Q: What’s changing with the MMRV vaccine (measles, mumps, rubella, varicella)?
The committee voted to no longer recommend the MMRV combination vaccine for children under age 4. Instead, children will now receive two separate shots: one for MMR (measles, mumps, rubella) and one for varicella (chickenpox).
“Previously, we were allowed to offer both to parents and let them choose. At this point, they have recommended against that and actually recommended against funding that for patients with Medicaid, no insurance, or those covered by the Vaccines for Children program,” Dr. Griffin said.
This means families on these programs will likely no longer have access to the single combination shot — only the individual vaccines.
Q: Will kids still get protected from these diseases?
Yes. Kids will still get vaccinated, but instead of one shot, they’ll receive two injections.
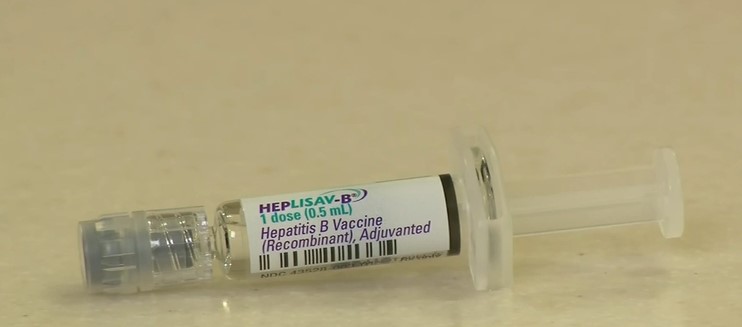
Q: What’s happening with the hepatitis B vaccine given at birth?
There are no changes for now. The committee chose to table discussion on any updates to the hepatitis B shot for newborns.
“Since we started giving it universally in 1991, we’ve seen cases in childhood drop from 18,000 a year down to 100 or fewer. When contracted at birth, about 90% of children go on to have chronic hepatitis B, which can cause liver failure and liver cancer,” Dr. Griffin said.
Q: Did the committee make any changes to COVID-19 vaccination guidance?
Yes — but not in the way many expected.
The panel rejected a proposal that would have required a prescription to get the COVID-19 shot.
Instead, they voted to shift toward individualized decision-making.
“In summary, they recommend that everybody discuss with their doctor if it’s right for you,” Dr. Griffin said.
Q: What does this mean for who should get the COVID-19 vaccine?
Under the new recommendation:
- Adults 65 and older: Vaccination based on shared decision-making with a health care provider.
- Individuals 6 months to 64 years: Vaccination based on individual risk — especially for those with underlying conditions or at higher risk for severe illness.
You do not need a prescription to get the shot, but providers are encouraged to counsel patients about whether the vaccine is appropriate for them.
Q: Are these changes final?
Not yet. The recommendations still need approval from the Acting CDC Director before they become official policy.
Q: Should parents be concerned about vaccine safety?
Dr. Griffin reassures families that the safety data hasn’t changed.
“There’s no new data suggesting these vaccines are unsafe. In fact, we have decades of science showing how safe and effective these vaccines are,” Dr. Griffin said.
She adds that if you have questions, talk to your child’s doctor.
“I wouldn’t recommend anything I wouldn’t do for my own family,” she said.
BOTTOM LINE FOR GREEN COUNTRY PARENTS:
- MMR and chickenpox vaccines will now be given as two separate shots for kids under 4.
- Hepatitis B at birth remains unchanged.
- COVID-19 vaccines remain available without a prescription, but individual decision-making is emphasized.
This story was written by News on 6’s MaKayla Glenn. You can view the full story online here.